Doctors for equality
 |
David Himmelstein and Stephanie Woolhandler are both distinguished professors at the School of Urban Public Health at Hunter College. In addition to having authored countless articles on health-care policy, they are also founders of Physicians for a National Health Program, which advocates for single-payer health insurance in the United States.
As the COVID-19 crisis unfolds in New York City and worldwide, people have been asking urgent questions about the flaws in our health-care system, and what can be fixed in light of this crisis.
To help answer some of these questions, Himmelstein and Woolhandler participated in Clarion’s “Five Questions” interview.
Hospitals worry about being overloaded. Why are hospital systems, many of which make lots of money each year, not able to expand their ability to provide more care?
There has already been some overall capacity expansion, and more is on the way. However, money can’t make new hospital resources appear instantly. Hospitals need spaces with ventilation systems that minimize contamination; plumbing in patient rooms so health workers can wash their hands and patients don’t have to wander the halls (spreading viruses) to use the bathroom; special mattresses that can be sanitized between patients; oxygen hookups or tanks available at each (or at least most) beds; computer stations where staff can access electronic medical records; ready access to diagnostic equipment like CT scanners; a call system that works at each bed, so patients can contact nurses if they need urgent help, etc. Useful, although less than optimal, hospital wards can be set up in convention centers, hotels, dorms etc., but hospital staff have little expertise in such construction or providing care in such settings, and lack in-house resources to undertake building construction or modification.
 |
Over the last several years, hospital ownership in lots of cities has been consolidated. University systems have bought up hospitals and clinics. How has this affected health care in America?
The giant systems that have taken over most hospitals and tens of thousands of physicians’ practices have used their monopoly power to leverage higher prices in negotiations with insurers. In the wake of mergers and acquisitions, hospitals’ profits have increased, but the availability of primary care and other services has decreased, and studies show that patients’ experiences have worsened and the promised quality improvements have not materialized.
In New York State, the per capita supply of hospital beds fell by 23% between 2000 and 2018, a slightly faster fall than occurred nationwide. Consolidation of ownership was partly responsible for the fall in hospital beds in New York, but the Andrew Cuomo administration’s explicit policy goal of reducing beds (particularly in New York City) was the main driver.
Do you think that this pandemic will inspire some sort of change toward something like Medicare for All?
The COVID-19 pandemic has highlighted the myriad weaknesses in our health-care and public health systems, and in our broader social safety net. Early diagnosis and isolation of infected individuals is key to stopping the spread of the virus, but the 29 million uninsured are largely excluded from care. Tens of millions more are saddled with steep copayments and deductibles, and restricted to their insurers’ narrow networks, obstructing their access to the care that’s a vital component of dealing with the epidemic.
In a recent survey, 68% of US adults said that high copayments and deductibles would discourage them from seeking care for coronavirus symptoms. Congress stepped in to make coronavirus tests free, but it did nothing to spare people who test positive from potentially disastrous medical bills for treatment.
The pro-market ideology that has dominated US health policy for a generation has also interfered with a timely and effective response. Those policies pit hospitals against one another as competitors and have pretty much abolished overall health planning that could assure that medical resources are distributed according to needs.
For decades, hospitals have amped up their provision of profitable services like elective orthopedic surgery, while neglecting unprofitable services like emergency care and mental health, and we have a concentration of resources in wealthy areas of Manhattan, while many parts of New York are underresourced.
We’ve also underinvested in public health, a reflection of the general assault on public services. The share of overall health spending devoted to public health efforts in the United States peaked at 3.21% in 2002, falling to 2.65% in 2016 (about half the level in Canada or the UK), and fell further to 2.45% in 2019.
Funding for the Centers for Disease Control and Prevention’s (CDC) Public Health Emergency Preparedness program, the main source of federal support for state and local public health emergency capacity, fell by one third between 2003 and 2019. These and other funding cuts forced state and local public health agencies to eliminate 50,000 positions, a 20% decrease in the frontline workforce for fighting epidemics. Similar cuts have affected the CDC as a whole, whose program funding, adjusted for inflation, decreased by 10% between the fiscal years 2010 and 2019.
These glaring failings offer opportunities for Medicare for All advocates to make the case for universal health care based on cooperation, solidarity and planning, rather than on competition and profitability.
Nurses’ unions have been vocal about the importance of a single-payer system. In this crisis, what can health-care unions do to inspire major change?
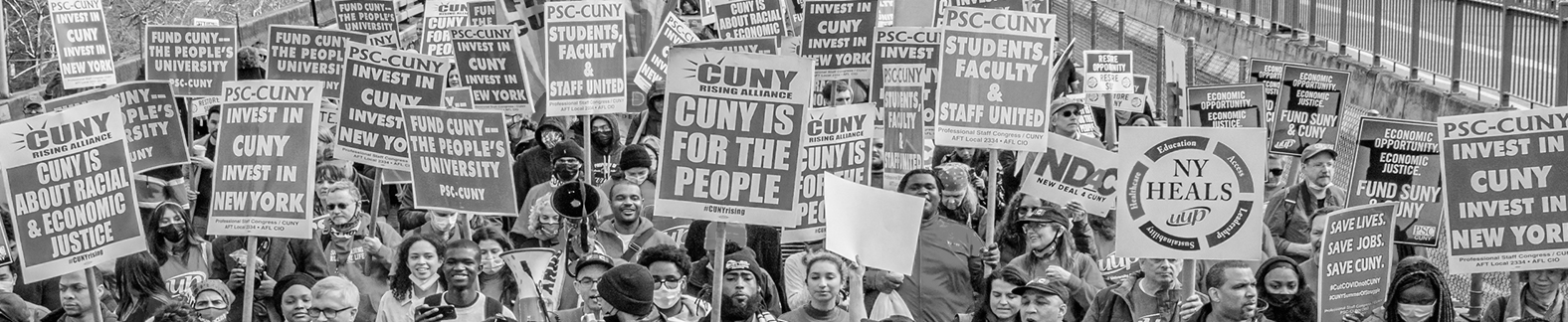
Broad popular mobilization will be needed to overcome opposition to a single-payer healthcare system by drug firms, insurers and other corporate interests that now reap enormous profits from the current dysfunctional system. Unions can be a vital force in sparking that mobilization through education and public advocacy. Health-care unions (as well as physicians) have a particularly important role to play in assuring the general public that single-payer reform would strengthen, rather than undermine, health care and that the health-care workforce would welcome such reform.
Italy is in a crisis, but Asian countries seem to be flattening their curves. What models should we be looking at?
Public health efforts and restrictions on movement and interaction have been key to stemming the COVID-19 epidemic in several Asian nations. When spread goes unchecked, no health-care system has the spare capacity to meet all the needs. So social distancing and identifying all of those who are infected and isolating them are critically important.
The most successful efforts have employed measures that impinge on freedom and privacy. While those measures save lives in the short run, they pose long-term threats. In the United States, we need to insist that any expansion of government’s surveillance powers and limitations on movement be immediately rescinded once the epidemic subsides.