In the past several decades, advances in prescription medications have cured diseases that had been incurable, relieved pain that once had to be suffered, and controlled the symptoms of many chronic conditions. The increased efficacy of pharmaceuticals has kept people out of the hospital, living longer and living more active lives.
At the same time, while prescription drugs are marketed as simple cure-alls, they are not. Some drugs are easy to administer and have very few side effects; some are exactly the opposite, with the cost to the body potentially outweighing the benefit. Some don’t work very well at all, or are effective for certain people but useless for others. Some drugs can be powerfully addictive, even when used as advised.
Big Pharma
Yet studies have shown a majority of patients consider a visit to a physician to be a failure if it doesn’t result in at least one prescription for their ailment. There is an ever-increasing belief that drugs exist to cure or relieve almost anything. That belief is magnified by $27 billion a year in drug company advertising.
“Big Pharma” is not altruistic, of course. Drug companies are in business to generate the maximum possible profits, and that goal shapes their decisions on how money will be spent. A 2012 paper in the British Medical Journal (BMJ) concludes that pharmaceutical corporations spend $19 dollars on marketing for every dollar they spend on research and development.
Profitability also determines how the research dollars themselves are used. Diseases that mainly affect the world’s poor people, like malaria, get little attention. But chronic diseases like hypertension, common in wealthier countries, are high research priorities: a chronic condition can generate years or even decades of repeat business.
Small Differences
“[P]harmaceutical research and development turns out mostly minor variations on existing drugs,” the BMJ authors note. “Sales from these drugs generate steady profits throughout the ups and downs of blockbusters coming off patents.”
Of course, the drugs that get the heaviest promotion are those that are the most profitable – not the most effective.
To sell a drug to consumers, a company needs to demonstrate to the FDA that the product performs better than a placebo – but it may perform worse than drugs already on the market. An art form has developed in setting up clinical trials that can find some niche that otherwise identical medication can’t claim, providing a technically accurate basis for competitive advertising claims.
You’ve seen countless ads for prescription drugs and they generally look the same: healthy, attractive people enjoying their lives in sunny settings. Millions of dollars are spent to generate the impression that a given drug – still under patent and highly profitable – is superior to lower-cost alternatives, even when its actual advantages may be slim to nonexistent.
An enlightened 2004 exposé, The Truth About the Drug Companies by Marcia Angell (former editor of the New England Journal of Medicine), provides some relevant examples. For instance, an eight-year study examined the effectiveness of three types of hypertension drugs, comparing the newer calcium channel blockers and ACE inhibitors with one that is tried-and-true (a diuretic). Considerably cheaper, a diuretic such as hydrochlorothiazide worked as well or better in most cases with fewer side effects.
Angell’s book details the failure of legislative efforts in the 1980s and 1990s to contain costs, with the National Institute of Health (NIH) in 1995 essentially abandoning its policy of insisting on “a reasonable relationship between the pricing of a licensed product, the public investment in that product and the health and safety needs of the public.”
Note that drug ads, unlike those of almost any other industry, don’t mention price or affordability. Most doctors are unaware of large cost differences among drugs that are identical or highly similar. (Meanwhile 90% of drug company advertising is directed at doctors.) There is essentially no limit on what can be charged the end user, with the result that drugs in the United States cost far more than in any other nation. Medicare is in fact banned by law from using its bargaining power to bring drug prices down.
The pricing for many new drugs, such as the large-molecule biologics dubbed ‘specialty’ medications, has been set at a level so high that companies don’t even try to claim that it’s all just to pay for research and development (R&D). The newest rationale for excessive pricing is that it factors in the savings in medical and hospital costs that can now be avoided!
Time for a Change?
With some medications now sold – in the US reaching $1,000 a pill, calls for a different model are growing. “Why can’t we have a system that ensures that research and development is paid for without needing to recoup those costs through high prices – most of which is not plowed back into R&D?” asks Brook Baker, a professor at Northeastern University.
Baker “favors an idea gaining currency among critics called delinkage, in which governments support pharmaceutical R&D as a public good,” reports National Public Radio. Drugmakers would “largely confine themselves to manufacturing, marketing and distribution” – with a likely drop in their outsized profits. (Publicly funded research is already a key part of drug development today, but that is forgotten when drug prices are set.)
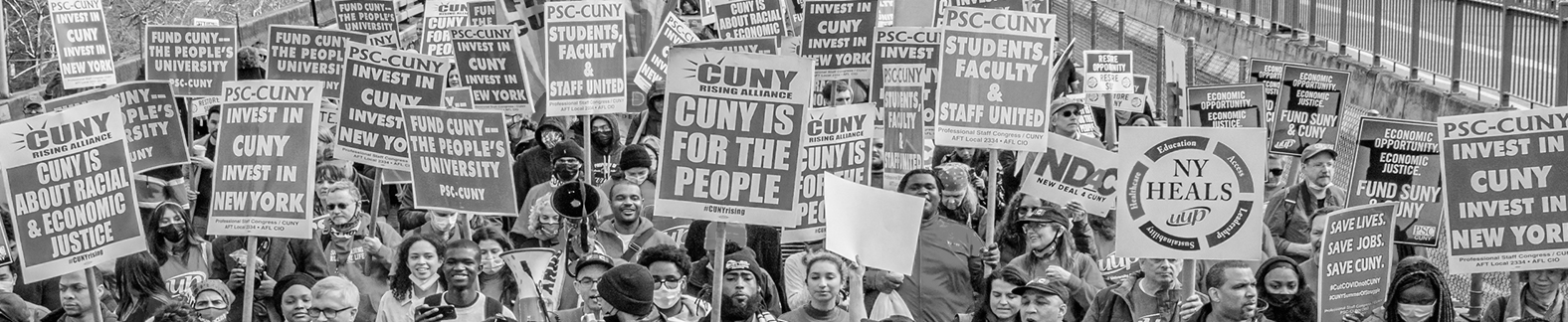
In the absence of serious reform, benefit providers like the PSC-CUNY Welfare Fund must act to counter Big Pharma’s predatory practices. That means ensuring, if an expensive medication is going to be prescribed, that the money is in fact providing particular benefit to the patient, and not just boosting drug company profits.
The Welfare Fund’s policies, such as having a formulary of medications, aim to make sure that the Fund’s limited resources are used effectively, so that your medical needs are met both today and in the future. The Fund recently announced some new rules toward that end (see below). Such controls on coverage can be an inconvenience, but they are a way to make sure that, at some point in the process, someone asks, “Is this expense necessary?”
When it comes to drug sales, we know this is a question that Big Pharma will never ask.
______________________________
RELATED COVERAGE